In today’s competitive healthcare landscape, managing costs effectively is crucial for the sustainability of healthcare benefits for an organization and its employees. The budget process, encompassing everything from forecasting to allocation, is a cornerstone of financial health. For companies self-funding their health insurance plan, this process is even more important. While the budget process might seem straightforward on the surface, it’s often fraught with complexities that can impact both the financial health of the organization and the quality of benefits offered to employees. It’s time to grow your budget!
The Challenges of Self-Funded Healthcare Budgets
As you crunch numbers and prepare your 2025 budget, healthcare spending can be one of the more difficult line items to predict for numerous reasons:
- Rapidly Evolving Healthcare Costs: Healthcare costs continue to rise at a significant rate, making it difficult to accurately predict future expenses.
- Unpredictability of Needs: While past data is helpful, illness and injury cannot always be planned for and may be more serious than expected.
- Regulatory Changes: The healthcare industry is subject to frequent regulatory changes, which can impact both costs and compliance requirements.
- Emerging Healthcare Trends: New technologies, treatments, and care delivery models can introduce both opportunities and risks to the budget.
- Data Complexity: Analyzing and interpreting complex healthcare data can be time-consuming and challenging for organizations without specialized expertise.
Enlist Help to Find Lost Dollars and Grow Your Budget
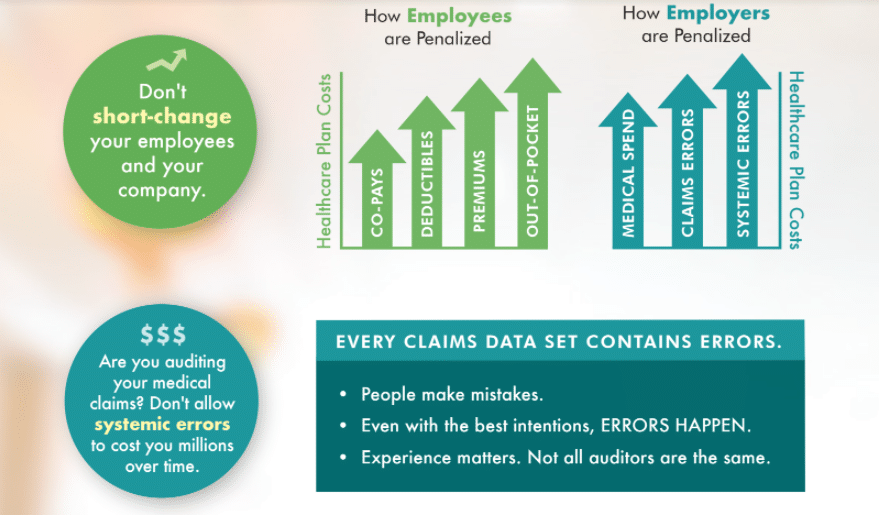
While benefits managers may have a strong understanding of their organization’s needs and the history of their plan, they may lack the specialized knowledge and tools required to navigate the complexities of self-funded healthcare budgets for the reasons mentioned. Partnering with a professional benefits consultant can provide the expertise and support needed to ensure the sustainability of healthcare benefits and protect – or even grow – the healthcare plan budget. One tool to achieve this goal is a healthcare claims audit.
Healthcare claims audits ensure accuracy, identify potential fraud or abuse and recover overpayments tied to employer healthcare plans. At Healthcare Horizons, we use a comprehensive audit method to track every claim and recover the most dollars possible. Our experienced auditors are adept at recognizing the red flags in a healthcare data set that may indicate an overcharge, systemic error (one that keeps repeating and snowballs into huge losses) or fraud. Once a claim is flagged as suspicious, we begin the process of working with the third-party administrator to correct the mistake. Once all parties agree the issue has been properly identified, the overpaid dollars are returned to the plan’s bottom line.
Healthcare claims errors typically range from 1 to 3 percent of total claims and can cost employers hundreds of thousands of dollars annually. That is a substantial piece of a budget.
Don’t Miss Out on Funds in Your Next Budget
Healthcare claims audits are an excellent tool to protect your self-funded healthcare plan. However, this strategy is most effective when combined with a solid service agreement with your third-party administrator. We will also review your current service agreement to ensure that it includes full audit rights. Limited (such as random sample audits) audit rights mean you can’t control what is analyzed – or how much money you may be entitled to have returned.
By leveraging the insights and tools offered by professionals, organizations can make informed decisions, optimize their budgets and protect their financial health in the face of an ever-changing healthcare landscape.