 The SHRM conference in New Orleans this year was spectacular (ending the event with a Brad Paisley concert was icing on the cake!). It was wonderful talking with friends in the Human Resources world – in person – and meeting many benefits managers eager to find ways to contain costs in their employee benefits plans. In listening to these HR professionals, we learned three things:
The SHRM conference in New Orleans this year was spectacular (ending the event with a Brad Paisley concert was icing on the cake!). It was wonderful talking with friends in the Human Resources world – in person – and meeting many benefits managers eager to find ways to contain costs in their employee benefits plans. In listening to these HR professionals, we learned three things:
- Most benefits managers think their brokers or TPAs handle all the auditing of their healthcare plans.
- Some were unaware that they should be reviewing audit rights in the ASO agreements.
- All worry about how much work it would be for them to do an audit and how much stress it would cause them.
Don’t Assume Your TPA is Looking Out for You
Your third-party administrator is tasked with one job: to process your medical claims in the most efficient manner. As benefits managers for self-funded employers, you trust your TPA to process the healthcare claims correctly so that you are not overfunding healthcare payments.
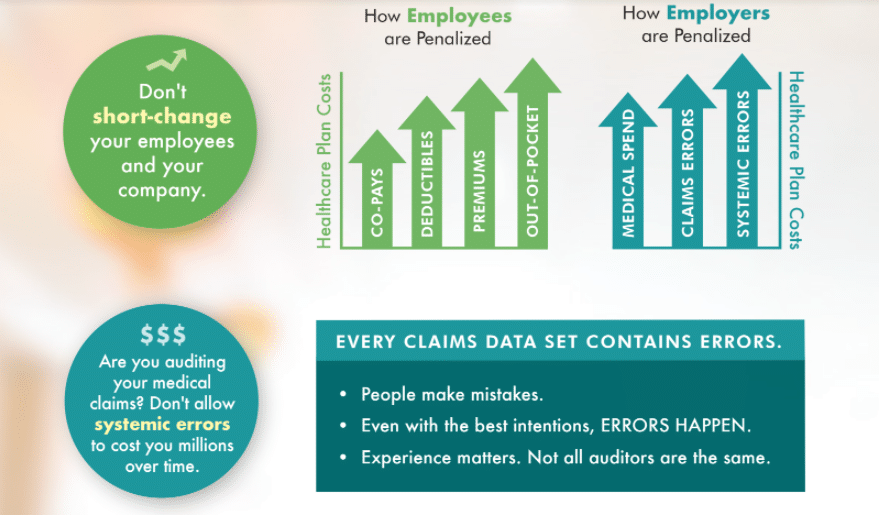
Unfortunately, even though so much of the process is automated, humans are still involved in the process. And humans make mistakes. Mistakes fall into one of two broad categories: one-off or systemic. (You can see a more detailed breakdown of the types of errors in our recent blog: Mistakes happen. Ignoring them could cost you.)
One-off errors are mistakes that, once fixed, shouldn’t happen again. These can include transposing a number in the claim code or misspelling a patient’s name. But just because these are “simple” mistakes, don’t think the financial hit can’t be significant! (Here is one example.)
Systemic errors are embedded issues within the claims process. These mistakes can cost a company hundreds of thousands of dollars over time. Typically, these errors occur because a mistake was made in setting up the plan. Examples include claims being filed through a location instead of a provider (as in this example) or a treatment being capped at a certain amount due to being categorized as out-of-network, when it actually is in-network.
The TPA has little incentive to look for these errors and recover overpaid monies. Why – because they are paying with your money not theirs. While most TPAs are excellent at what they do and truly do want to process claims mistake-free, it’s impossible to do so at 100%. In fact, estimates show that up to 80% of claims data has an error. Not all of these errors have a financial impact, but many do. If your TPA, through your service agreement, is telling you they will perform an audit and that they guarantee a 98% success rate, you should ask for more details. Is the audit a random sample selection of claims for review? If so, it is highly likely they won’t randomly select the claim with the mistake. Are you willing to take that chance?
Your Company Does Not Have to Settle for the Standard Audit Language
In any negotiation, the first offer is probably not the best. The same is true for the audit rights language in most TPA service agreements. While the agreement says that you have audit protection, the language is typically very restrictive. For instance, does the agreement say that you cannot work with an outside audit firm? Make sure you are negotiating for comprehensive, independent audits. Not sure what to look for? Read this blog for tips. Additionally, we offer a no-cost audit language assessment to determine the effectiveness of the audit system in place for your company.
HealthCare Horizons Does the Work for Benefits Managers
HR professionals are busy. Our audit process involves you as much – or as little – as you want. Once you set the process in motion by giving us access to your medical claims data, we only need to involve you to decide which claims you would like to pursue for recovery. We provide clear communication on the impact the recovery will make (hint: it isn’t just the amount of dollars reimbursed!) and we will work with your TPA to move forward. If there is a systemic error, we will also explain in detail where the breakdown in the setup occurs so that your TPA can correct the problem.
As for stress? The only stress involved will be if you DON’T have regular comprehensive audits. Now that you know that there are most assuredly mistakes in your data set, the idea of losing money that could be returned to your company’s bottom line will cause sleepless nights.
The Only Bad Mistake is the One You Don’t Address
We say it often, not finding mistakes will do more long-term harm to your company, and potentially your credibility, than having an audit discover errors. Finding the claims errors and recovering dollars from overpaid medical claims means more money for your company’s bottom line. As the benefits manager, that is your responsibility. That money can go toward other valuable programs within your organization. Not to mention the money you save employees. Now you know. So now is the time. Contact us to start your medical claims audit. Cause the Effect.