Have you ever had rabbits in your yard? One or two may seem harmless, but left unchecked, they will quickly multiply and destroy your landscaping, garden and grass, leaving you with a big bill to fix the mess. Systemic errors in a self-funded health insurance plan work the same way. One error that costs your company $100 won’t impact the bottom line significantly. But that same $100 error, committed numerous times over an extended period, will cost your company a lot of money…sometimes even millions of dollars!
How Systemic Errors Occur
Self-funded health insurance plans are popular for businesses, specifically those with a large number of employees, because they can lower costs, provide more flexibility on coverage and include greater control over benefits. However, because of their scope, self-funded plans can be more susceptible to systemic errors.
Systemic errors are mistakes that occur in the underlying systems and processes of a plan. They can be caused by a variety of factors, including benefit plan setup errors, incorrect coding edits, abusive or fraudulent billing, inadequate processor training and outdated technology.
Some of the most common systemic errors in self-funded health insurance plans include:
- Incorrect eligibility determinations, leading to employees being denied coverage or receiving incorrect benefits.
- Inaccurate claims processing, resulting in delayed or denied payments, or in incorrect amounts being paid.
- Fraud and abuse are intentional errors that occur when employees file fraudulent claims or providers bill for services that were not rendered.
The Fix for Errors is in Your Data
Employee complaints are one red flag that errors are occurring in your health insurance claims. Health insurance is an area that your employees need to trust will be accurate and available. When claims repeatedly are denied or employees must pay a larger than expected out-of-pocket share, there may be an unnoticed error in processing.
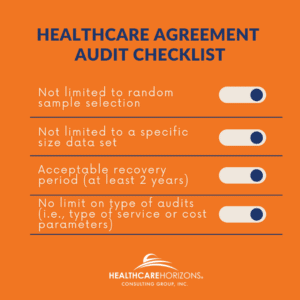
Finding those errors happens through a careful analysis of claims data sets. These reviews are done through audits. In our comprehensive audits, we work with you to audit your third-party administrator (TPA) and identify potentially incorrect claims. By analyzing complete data sets, and not just random samples, it is possible to identify patterns that suggest the presence of systemic errors (this also catches one-off errors!). For example, if a particular type of claim is consistently denied, this may indicate a code was incorrectly entered when the system process was set up. Once we flag suspicious claims, we collaborate with you – our client – to determine which claims to assess fully. Then we go to work to recover overpaid dollars and return them to you.
Systemic errors can be sneaky because when the error occurs it might not be noticed, either due to the smaller dollar amount error or confusion over medical claims language. This stealth behavior underscores the need for regular outside audits of your self-funded plan by experts. Only with regular reviews can you be sure that your plan is being administered correctly, employees are receiving their full benefits and your plan is not overpaying for care.
It’s time to get the rabbits under control. Contact Healthcare Horizons to begin managing your healthcare expenses with a comprehensive audit.